What Is The Most Effective Treatment For Fungal Nail Infections?
Representing half of all nail abnormalities in adults,2 fungal nail infections have long been a point of frustration for podiatrists during a clinical presentation. Wanting to offer the patients a solution, some clinics offer various anti-fungal topical creams and ointments. Others prefer referrals back to the GP for oral medications. Recently, both hot and cold laser have become a popular treatment, with practitioners beginning to offer this in their clinics or referring to clinics that have the available technology.
Given the emergence of new fungal toenail treatment, the growing pool of evidence, and the desire to ensure a podiatrists’ professional recommendations are justified, we’ve reviewed the available therapies for fungal nail infections against their ease of use, safety, compliance and efficacy so you can make an informed choice for your clinic.
Topical Ointments: Creams, Lacquers And Paints
Topical antifungals are those applied to the surface of the nail. The most common active agents here in Australia include morpholine, amorolfine and ciclopirox. Unfortunately, the anatomy of the nail impairs the ability of topical treatments to effectively penetrate the nail to reach all the fungus, with the concentration reported to reduce by 1,000 times from the outer to inner nail areas.3
Efficacy
Topical antifungals maintain a relatively low success rate of between 5.5% and 17.8%.4 When coupled with manual debridement of the nail by podiatrists, efficacy may increase up to 38%,5 but this has its limitations. Ciclopirox-based Rejuvenail, which claims to be Australia’s #1 anti-fungal nail brand based on sales, states that full cures can be expected in less than one in three people,6 assuming that the infection does not involve the lunula – the crescent-shaped area at the base of the nail. As many fungal nail infections do involve the entirety of the nail, the true success rates for patients seen in podiatry clinics may drop even lower.
Side effects
Most topical antifungals are not recommended for use in those aged under 18 years. They have a number of potential side effects that are typically localised, mild and short-lived. These include skin irritation, redness, scaling, burning, itching, discolouration of the nail and allergic dermatitis.
Ease of use
Topical antifungals require manual application directly onto the nails. This may pose a problem for those that cannot easily reach their feet, have vision disturbances, unsteady hands and more. Ease of use is further reduced if regular podiatric debridement is recommended to increase efficacy due to transportation, organisation and appointment cost.
Compliance
Topical antifungals are usually applied at least once a day, for a period of 9-12 months for toenails.7 This may make it difficult for patients to stay compliant when paired with the ease of use difficulties – and if only three in ten people are expected to see satisfactory results over a year of use.
Systemic Therapy: Oral Medications
Oral medications must be prescribed by a GP and are given as a tablet to be ingested, bypassing the nail barrier encountered by topical treatments. The most common active ingredients include terbinafine and itraconazole.
Efficacy
Both active agents have proven efficacy when studied against placebo treatments, with high-quality evidence.8 Mycological cure rates have been as high as 54-70% after 48 weeks of use, although complete cure rates in the same reviews were only found to be between 14-38%.9 Mycological cures are defined as eradication of the fungal pathogen from the nail as confirmed by a negative fungal culture and a KOH test, whereas a complete cure meets the goals of the patient, physician and regulatory bodies, defined as a 100% clear nail. It should also be noted that up to 20% of people are found to relapse within a few months of oral antifungal treatment.10
Side effects
For those that are vulnerable, the potential side effects and drug interactions of oral medications are perhaps the most significant. Itraconazole may enhance the effects of warfarin and oral hypoglycemics which are not uncommon in podiatric patients, as well as causing nausea, headaches and abdominal pain. Allergic skin reactions may also occur, with taste disturbances and hepatotoxicity also being reported with terbinafine use.12
Ease of use
As daily tablets, ease of use is high when memory is optimised, like when placed in an obvious place or alongside other daily medications.
Compliance
Due to the ease of use, we would assume that compliance would be fairly high. However, a study of 330 patients measuring compliance of oral antifungal use found that the overall compliance rate for patients on either itraconazole or terbinafine was only 55%. Of those that were not compliant, 29.73% were worried about the side effects of medicine, 22.3% thought that they had already been cured, 15.54% was due to economic reasons and 12.16% could not bear the side effects of the medicine.13
Laser Treatment
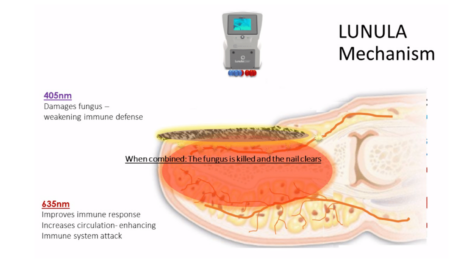
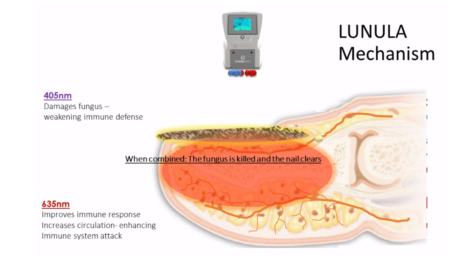
Laser treatment for onychomycosis falls into two distinct categories: hot laser and cold laser. Hot laser heats the nail to temperatures around 50 degrees,14 inhibiting the growth of the fungus, destroying it, and even helping to sterilise the area to help prevent new fungal growth.15 Cold laser, which is where the Lunula laser is leading the world, works by using two rotating laser beams simultaneously set to different cold frequencies. The first beam acts on fungus within the nail, nail bed and surrounding tissues, while the second works on the body’s natural immune response, helping to clear the fungus.
Efficacy
While the research base of this modern treatment is still building, both hot and cold laser have been found to have superior clearance rates in smaller-scale studies, ranging from up to 85% for hot laser 16,17,18 to up to 99% for cold laser.19,20 In a study of 323 patients undergoing cold laser, only four patients had a recurrence of their infection at 48 weeks. Given that onychomycosis has shown to have a relapse rate as high as 40–70%, these results are very promising.21 Laser efficacy has also been demonstrated in infections of mild, moderate and severe intensities.22
Side effects
Cold laser is reported to be completely safe with no temperature changes or other adverse effects, and is non-invasive. For hot laser, the need to significantly heat the nail can result in pain and occasional bleeding after treatment.23 To help offset these side effects and minimise patient discomfort, air cooling may be used during hot laser treatment.24
Ease of use
Both hot and cold laser are performed in-clinic. Hot laser is a hand-held treatment manually performed by the podiatrist one toe after the other, due to the sensitive nature of the heat. Cold laser is an automated process performed in 12 minutes per foot, automatically by the Lunula device, after foot placement and assessment by the practitioner. While the ease of use for the patient is the same, as Lunula is automated and treats the five toes at once, it has greater ease of use for the practitioner. Practitioners can then leverage the treatment time to discuss infection control protocols and home care advice with their patient – education that is essential for helping prevent recurrence.
Compliance
Both hot and cold lasers require weekly attendance at the clinic for approximately four weeks. While few studies have examined or made reference to compliance in return visits, we predict a relatively good compliance rate compared to topical or oral treatments due to the relatively low number of total visits paired with the financial investment into the treatment.
So Which Is The Best Treatment For Onychomycosis?
Given its superior efficacy, ease of use for both patient and practitioner, safety with no adverse effects, our top pick is the Lunula cold laser. As a clinic, alongside solving a common and frustrating problem for your patients, it also adds a fantastic revenue stream. See what your potential income versus outgoings could look like here.
If you’re unsure of how the laser could work in your clinic, you can take advantage of a free, no-obligation trial. For more information on the Lunula laser, including how it works and its research, click here.